|
|
|
Breathing Lessons |
|
Allergy writer Alex Gazzola discovers how breathing can affect allergies and sensitivities. |
|
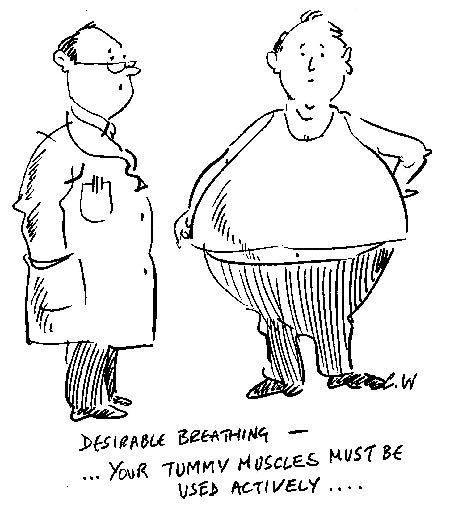
We inhale and exhale around twenty thousand times a day, but according to some experts, incorrect breathing can trigger or worsen the gastro-intestinal, food intolerance and food allergy symptoms most of us would much prefer to live without. So is it time for those of us with food sensitivity issues to take a close look at how we take in our air? Jen Tiller of Reality Quest is a complementary therapist and Buteyko practitioner who reduced the severity of her food sensitivities by doing just that. She says that all of us are born with the innate ability to ventilate ourselves appropriately, but that bad breathing habits are easy to pick up in life, leading many of us to breathe wrongly – from our chests, rather than from our abdomens, using our diaphragms. The end result is hyperventilation – breathing more than we need to breathe. She adds: ‘Often it’s a cumulative effect. You might have a virus, perhaps an emotional upset, you may start to eat poorly, and your body lapses into poor breathing. Our default position is correct breathing, but so much can throw it out of kilter, that you need to make a conscious decision to restore it.’ ‘Your tolerance to alcohol will also be very low – and this is a possible sign that you’re hyperventilating,’ she adds. ‘If you used to be able to handle a glass of wine but can’t now, for instance, or one glass feels like three or four and leaves you with a hangover, this could be an indication of poor breathing.’ Breathing solutions There is a simple technique to gain an awareness of your breathing, and it serves as a useful regular exercise to encourage healthy breathing in the long-term. It’s a good idea to ‘check’ your breathing periodically, much as you might check your posture for slouching. Taking up yoga, meditation or related disciplines helps – as much of the benefits derived from these will be breathing-related. She adds: ‘Obviously, I don’t recommend taking unnecessary risks, but reactions will probably be milder as you address your breathing, and if asthma and wheezing are factors, controlled breathing with pauses will reduce these symptoms, and keep you calmer, which is of huge value during an allergic reaction.’ ‘If you habitually hyperventilate you are putting constant stress on many of the body’s systems,’ summarises Jen. ‘If you can address that, it takes such a burden off the rest of the body that problems will resolve themselves, and you will have huge benefits to your health and well-being.’ Useful Information First published in 2008 More articles on the management and treatment of food allergy and intolerance |